Are You in a High-Risk Group?
Black, Indigenous, People of Color (BIPOC), pregnant women, individuals with chronic conditions, and those over the age of 65 have been among the hardest hit by the pandemic. Many in these high-risk categories have questions about COVID-19 vaccinations, particularly given misinformation distributed through social media and a history of past government and medical transgressions against people of color. It is important to establish trust in the COVID-19 vaccines and the vaccination process if we are to overcome this pandemic.
Your Vaccination Guide will be able to answer your questions and give you the tools you need to make an informed decision. Over one million people have died in the U.S. alone from COVID-19. That is about 15 Super Bowl stadiums full of people. Vaccines are saving lives. Will you get the shot and boosters so you are alive to watch the next Super Bowl, attend a family marriage, greet the birth of a baby, or do something that means so much to you, your friends, and your family?
Quick Links
Chronic Health Issues | Health Equity Issues | Being Over 65 | Pregnancy | Other Health Issues
Chronic Health Issues Place You at Higher Risk
A chronic disease or condition can stay with people for all or most of their lives and places individuals at greater risk for harsh effects from COVID-19. Half of all American adults have at least one chronic condition, and almost one in three have multiple chronic conditions (CDC).
Having any chronic condition, no matter your age, places you at greater risk from COVID-19. If you have a chronic condition, visit the CDC website for information about specific conditions or one of our partner sites to reach those informed about that condition. You also likely want to know if you should get the vaccine.
Can People with Chronic Health Conditions Get the Covid-19 Vaccine?
Yes, people with chronic conditions can get the vaccine (CDC). It is important, however, to talk to your doctor to find out if you should get the vaccine particularly if you have a compromised immune system or had an earlier reaction to a vaccine. Check with your doctor regarding the specific vaccine you are scheduled to receive. Visit the California Chronic Care Coalition for more information related to chronic disease or My Patient Rights if you have trouble accessing care.
Were the COVID-19 Vaccines tested on people with chronic conditions?
In the Moderna vaccine trial, 22.3 percent of participants had at least one high-risk condition, which included lung disease, heart disease, obesity, diabetes, liver disease, or HIV infection. Four percent (4%) of participants had two or more high-risk conditions (CDC). The Pfizer vaccine trial included people with obesity (35.1%), diabetes (8.4%), and pulmonary disease (7.8%).
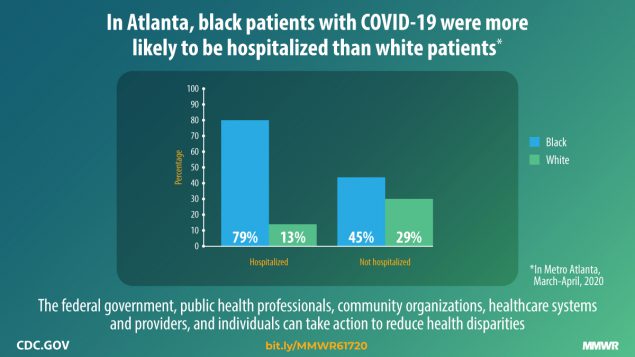
BIPOC Population at Higher Risk
Black, Indigenous and Persons of Color (BIPOC) come from many different backgrounds, cultures, lived experiences, some of which have increased vaccine skepticism. Unfortunately, statistics show that these groups are also among the most at risk from COVID-19.
More statistics related to COVID-19 can be found on the CDC website.
The good news is there is a vaccine to keep you safe. Many people are hesitant or afraid to get vaccinated. Black people in particular have been subjected to what amounted to experimentation in the past. Historical experiences with research abuses have established doubt and skepticism about the trustworthiness of science, research institutions, and government that are not easily overcome.
Moving from vaccine hesitancy to trustworthiness through dedicated community engagement must be a top priority. Ongoing challenges prompt an urgent need to address the inequities in access proactively to avoid turning the vaccine rollout into one more example of ongoing unfair treatment. Building relationships within your community requires actively listening to others’ stories and ensuring that all partners are provided an opportunity to articulate the challenges, barriers, and facilitating factors they have encountered (NEJM).
The government and healthcare providers have become more aware of health inequities and claim to be doing their best to provide a more equitable distribution with concentrated plans to reach and offer vaccinations to areas and people traditionally underserved.
Let’s address some of your concerns.
Wasn’t the Vaccine Created Too Fast? Are We Guinea Pigs Again?
Some have expressed concern that the vaccines were created, investigated, and approved too quickly. All Americans should be assured that FDA processes and normal safety protocols were followed, but at a more rapid pace because of the need to get the pandemic under control and avoid unnecessary delays. The FDA continues to monitor on going trials and track vaccine use and results. Visit the COVID-19 page of this website for more details.
No one has been viewed as guinea pigs in distributing the vaccine. Medical professionals across the country generally received the vaccines first to demonstrate vaccine safety and to ensure their protection as they treat COVID-19 patients. Millions of vaccines have already been administered with relatively few problems (CDC).
Is it Safe for BIPOC to Take the Vaccines?
It may be helpful to note that the vaccine trials included Black, Indigenous, and People of Color. The Moderna vaccine had 20% Hispanic/Latino, 9.7% African American, 4.7% Asian, <3% other races/ethnicities (CDC). The Pfizer vaccine included: 26.2% Hispanic/Latino, 9.8% African American, 4.4% Asian, <3% other races/ethnicities (CDC). The Johnson & Johnson vaccine trials included 62.1% White, 17.2% Black or African American, 8.3% American Indian or Alaska Native, 5.4% Multiple races, 3.5% Asian, 0.3% Native Hawaiian or other Pacific Islander participants (CDC). Learn more about the specific vaccines on the COVID-19 Vaccines page of this website. However, if you have health conditions or have had previous reactions to vaccines, you should talk to your doctor before getting vaccinated. Read this page regarding health issues and getting the vaccine.
There are ways to increase your comfort in getting vaccinated. You may go to any convenient location where you are comfortable or consult your doctor. For your health and your family’s health, please consider getting vaccinated. The CDC has a page that may answer additional questions you have.
Is Language a Barrier to Receiving Care or the Vaccines?
Understanding the need for COVID-19 safety steps, receiving treatment, and getting vaccinated may be affected by a language barrier, but it is possible to find a doctor, or doctors with office staff, who can speak your language. An increasing number of vaccination information and registration sites are available in multiple languages. Some vaccination locations will have options for non-English speakers. Contact your local health department or your doctor’s office to find resources to address language barriers.
Should You be Concerned About Going to Get a Vaccine if You Are Not a U.S. Citizen?
Noncitizens and immigrants can get the vaccine. Health workers should not ask you for citizenship status when you get a vaccination. They will ask questions to determine if you should be getting a vaccine at that time such as how old you are (your birth date) and if you have any health issues. The vaccine is free. No one, including non-citizens, will be charged for getting a COVID-19 vaccine.
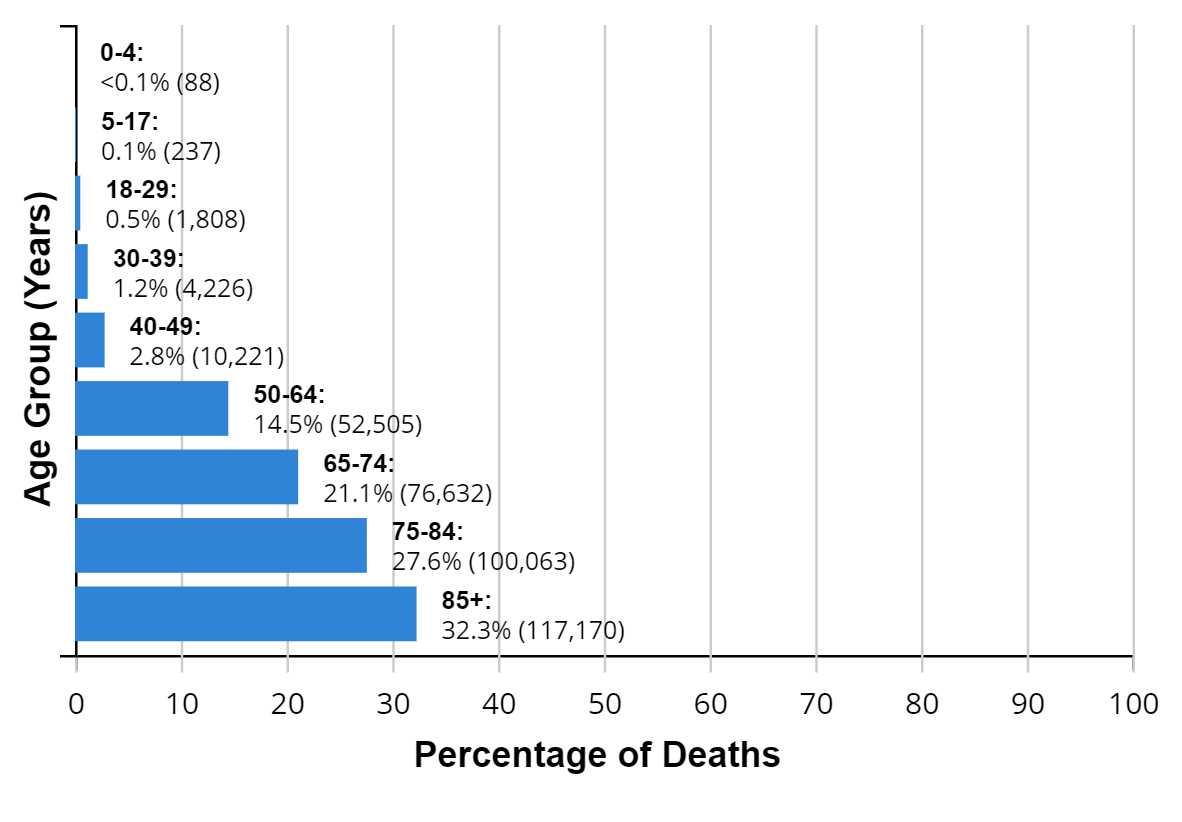
Your Age Can Put You at Increased Risk
If you are over 65, you are in the high-risk group for COVID-19. As we age, we tend to have more health challenges and those can increase your chances of getting COVID-19 and other infection risks. The federal government and most states have prioritized 65-and-older individuals to be vaccinated. The CDC chart below illustrates the increased death rates from COVID-19 as we age.
COVID-19 statistics by age on the CDC website.
Are You Concerned About the Cost of the Vaccine?
The vaccine is currently free to everyone. Visit the Vaccine Cost page on this website if you want to know more about the cost of vaccines.
Pregnant Women
and Risks Related to COVID-19
It turns out that pregnant women are not any more likely to get COVID-19 than anyone else. However, they are more likely to become seriously ill if they do get it. They could also have “adverse” pregnancy outcomes such as early birth as compared to pregnant women without COVID-19 (CDC).
Are Pregnant Women Able to Get the Vaccine?
Pregnant women were not in the original trials of either the Pfizer, Moderna or Johnson & Johnson vaccines, so available data on the success of the vaccines on pregnant women is limited. However, the World Health Organization says that “based on what we know about this kind of vaccine, we don’t have any specific reason to believe there will be specific risks that would outweigh the benefits of vaccination for pregnant women.” Pfizer began including pregnant women in a trial at the beginning of 2021.
Pregnant or breastfeeding women at high risk of exposure to the COVID-19 virus, such as health workers, or those with additional health issues which add to their risk of severe illness, should consult with their healthcare provider about being vaccinated.
Other Diseases that Put You at Increased Risk
Ver esta página en español